Effects of postpartum depression on child development
Effects of Postpartum Depression on Child Development
Disclaimer: This article is a thesis review or a postpartum depression research paper on the topic, "Effects of postpartum depression on child development at Dodowa Hospital, Ghana"
Researcher: B. B.
Introduction
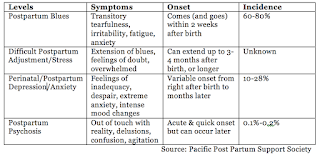
Post-partum depression (PPD) is one of the
world’s increasing epidemics. The American Psychological Association (APA) estimates 9-16 per cent of
postpartum women experience PPD. Among women who have already experienced PPD
following a previous pregnancy, prevalence estimates may increase to 41 per cent
(APA, 2012). Stuart-Parrigon &
Stuart (2014) observes that approximately between 11-42 %
of women experience postpartum depression globally. Introduction
Although the rates vary across regions, depending
on socioeconomic status and other determinants of health such as access to
quality of health care, PPD can cause grave health implication for both mother
and child. The condition has been found
to produce increased risk
for anxiety, cognitive impairment, guilt, self-blame, and fear in mothers,
thereby hugely interfering with their ability to function in everyday life. Children
of mothers with PPD may become withdrawn, irritable, or inconsolable, and display
insecure attachment and behavioral problems (Steward, Robertson, Dennis,
Grace and Wallington, 2003).
Main Objective
The aim of the study was to determine the
level of knowledge with regard to the effects of postpartum depression on child
development among women attending postnatal clinic at Dodowa Hospital and how
this may be affecting the children they are raising with respect to their
development.
Rationale
Postpartum
depression has been found to impact child development (Stuart-Parrigon &
Stuart, 2014). The phenomenon has several health implications for mothers,
children and sometimes even men, who by various indications within African
cultural perspective are less involved in the complications of childbirth. Research
conclusions have noted an association between the postpartum period
and mood disturbances (Miller, 2002). Other studies have linked the condition
to grave affective disorders (Nonacs & Cohen, 1998).
Key Findings
Largely, women visiting
Dodowa Hospital are adequately aware of postpartum depression. However, the strongest
misconception amongst the respondents was the notion that witchcraft is responsible for PPD; whereas, the weakest misconception was the notion that PPD was caused by
bacteria.
The most
important risk factor that predisposes women to PPD is Personal or family history of depression, followed by acute stressors. The least important
risk factors that predispose women to PPD are changes in hormonal levels and giving
birth early (young motherhood).
PPD seems to have the
greatest effect on the following components of child development: the child’s physical and creative play at
school, followed by the bonding
between mother and her infant and
level of intelligence of the child. However, there was no significant
difference in the effect of PPD amongst the following components of child
developments: early interaction, cognitive and linguistic development,
and behavioural and emotional development.
Abstract
Post-partum depression (PPD) is one of the
world’s increasing epidemics. Postpartum depression refers to a kind of
depression experienced by some women mostly after childbirth. In fact, postpartum depression has been found to impact
child development. Additionally, knowledge about PPD may rather be on the low
side. This study therefore sought to investigate the effects of postpartum
depression on the development of children of postpartum mothers, as well as an
examination of the level of awareness and misconceptions women have of postpartum
depression. The study was essentially descriptive in nature and employed the
empirical research design. Primary data was collected by questionnaire
administration.. The research setting was Dodowa District Hospital. The strongest
misconception amongst the respondents was the notion that witchcraft is responsible for PPD. Such was the strength of this
misconception that many of the respondents when asked how they will tackle PPD
said they will seek spiritual help or guidance. Low level of education of
majority of respondents may have affected the way information disseminated was
perceived, thus leading to misunderstandings and misinterpretations, which
eventually led to misconceptions. The most important risk factor that
predisposes women to PPD was found to be Personal or family
history of depression, followed by acute stressors.
Indeed,
19 out of the 50 respondents, representing a massive 38 %, have one time or the
other had thoughts of harming themselves. This means that for every 10 persons
that visit the Dodowa hospital, at least
3 of them have suicidal thoughts. This explains the strong agreement of the
effect of PPD by respondents on their infants. The effects of PPD seem to be greatest on the behavioural and emotional development of
the child. It is recommended that postnatal classes being organized by
the Hospital for postpartum women should be geared more towards addressing some
of the misconceptions held by postpartum women about PPD.
Some References
Abou-Saleh, M. T., Ghubash, R., Karim, L.,
Krymski, M. & Bhai, I. (1998). Hormonal aspects of postpartum depression. Psychoneuroendocrinology, 23(5),
465-475.
Abell, S. (2007). Postpartum Depression. Clinical Pediatrics (Phila), 46, 290-291.
Affonso, D. D., De A. K., Horowitz, J. A.
& Mayberry, L. J. (2000). An international study exploring levels of
postpartum depressive symptomatology. Journal
of Psychosomatic Research, 49, 207– 216.
Akhtar, N., Dunham, F. & Dunham, P. J.
(1991). Directive interactions and early vocabulary development: The role of
joint attentional focus. Journal of Child
Language, 18, 41-49.
American
Psychiatric Association. (2013).
Diagnostic and Statistical Manual of Mental Disorders,
Fifth Edition (DSM-5).Arlington, VA: American Psychiatric Association.
American Psychological Association. (2015).
Postpartum Depression. Washington, DC.
Appleby, L., Warner, R., Whitton, A. &
Faragher, B. (1997) A controlled study of fluoxetine and cognitive-behavioural
counselling in the treatment of postnatal depression. British Medical Journal, 314(7085), 932-936.
Areias, M. E., Kumar, R., Barros, H. &
Figueiredo, E. (1996) Comparative incidence of depression in women and men,
during pregnancy and after childbirth. Validation of the Edinburg Postnatal
Depression Scale in Portuguese mothers. British Journal of Psychiatry, 169(1),
30-35.
Bågedalh-Strindlund, M. & Monsen-Börjesson,
K. (1998). Postnatal depression: a hidden illness. Acta Psychiatr Scand, 98: 272-275.


.webp)







hi. can i use this image for making ppt poster presentation competition
ReplyDelete